Sarah had been caring for her mother at home for three years after her Alzheimer's diagnosis. She'd cut back her work hours, stopped seeing friends, and hadn't taken a vacation since 2022. When her sister offered to watch their mom for a weekend so Sarah could attend a friend's wedding, she broke down crying. "I can't leave her with you for two days," she said. "She wanders at night. She gets confused with new people. What if something happens?" Her sister suggested trying a week of respite care at a local memory care community. Sarah reluctantly agreed, expecting to feel guilty the entire time. Instead, she slept through the night for the first time in months. When she picked up her mom a week later, the staff showed her how much calmer her mother seemed with professional dementia care and consistent routines. That's when Sarah started asking questions about permanent placement.
This scenario plays out in thousands of families every year. Respite care and memory care serve different purposes, but understanding both options helps you make better decisions about your parent's care and your own wellbeing.
Understanding the Two Types of Care
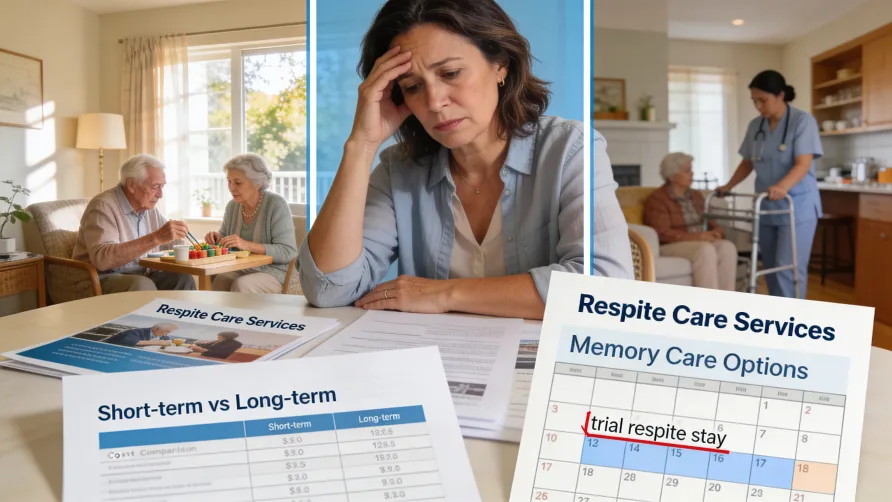
Respite care provides temporary relief for family caregivers. You arrange coverage for a few hours, days, or weeks while you rest, handle other responsibilities, or simply step away from constant caregiving. Your parent receives professional care during this time, then returns home when the respite period ends.
Memory care offers permanent residential support specifically designed for people with Alzheimer's disease and other forms of dementia. These specialized communities provide 24-hour supervision, secured environments to prevent wandering, and staff trained in dementia care techniques. Residents live there full-time rather than returning home after a short stay.
The key difference is duration and purpose. Respite gives caregivers a break. Memory care addresses the ongoing, escalating needs of someone with progressive dementia who can no longer be safely cared for at home.
Short-Term Respite Options
You can access respite care through several settings, each with different timeframes and support levels.
In-home respite brings a professional caregiver to your house for a few hours or overnight. This works well for shorter breaks like attending appointments, running errands, or getting a full night's sleep. Your parent stays in familiar surroundings, which can reduce confusion.
Adult day programs offer daytime supervision and activities, typically from morning until early evening. Your parent attends the program several days per week while you work or handle other responsibilities. Most programs provide meals, social activities, and basic health monitoring.
Facility-based respite provides overnight stays at assisted living communities, nursing homes, or memory care facilities. Stays usually range from a few days to several weeks. This option offers 24-hour professional care and gives family caregivers extended relief, whether for vacation, medical recovery, or managing caregiver burnout.
Some memory care communities offer respite stays specifically for people with dementia. These short-term placements allow families to try memory care before committing to permanent placement.
When Respite Becomes Permanent
What families often underestimate is how frequently respite care serves as an unintended trial run for permanent placement. You book a week of respite thinking you'll bring your parent home, then realize the arrangement works better than you expected for everyone involved.
The transition happens in predictable patterns. Your parent adapts to the professional care environment faster than you anticipated. Staff members trained in dementia care spot needs you've been struggling with at home. The secured environment prevents wandering incidents that terrified you at 2 a.m. Your parent participates in structured activities instead of sitting alone while you work. When the respite period ends, you face a difficult truth: returning home might not be the best option anymore.
Staff at memory care communities report this scenario frequently. A family books respite care for two weeks while the primary caregiver recovers from surgery. During visits, they notice their parent seems calmer, more engaged, better rested. The staff mentions behaviors they've managed successfully, issues the family has wrestled with for months. By week two, the conversation shifts from "when can Mom come home?" to "what would permanent placement look like?"
Several factors drive this shift. Caregiver exhaustion becomes undeniable once you experience relief from constant responsibility. Many caregivers don't realize how depleted they've become until they sleep through the night, leave the house without anxiety, or simply have time to think clearly. The respite break reveals the true cost of home caregiving on your health, relationships, and quality of life.
Safety concerns surface during respite stays. Professional staff document wandering attempts, aggressive behaviors during personal care, medication refusals, or fall risks that family members have been managing through constant vigilance. What seemed manageable at home looks different when professionals show you the level of supervision truly needed. You realize you've been providing skilled nursing oversight without training or backup support.
Your parent's response to professional care provides compelling evidence. Some people with dementia resist care from family members but accept help from trained staff. The role confusion dissolves when professional caregivers provide assistance. Your parent may participate more readily in bathing, dressing, and meals when family dynamics aren't tangled up in the interaction. Memory care staff use specialized techniques you haven't learned, approaching challenging behaviors with methods that reduce resistance.
The structured environment benefits many people with dementia. Consistent daily routines reduce confusion. Regular meal times, activity schedules, and sleep patterns help regulate behavior. Secured outdoor spaces allow safe walking without elopement risk. Social interaction with other residents provides stimulation that isolated home care can't match. Your parent might actually thrive in ways you didn't think possible.
Financial realities become clearer during respite care. If you've been paying for home health aides, adult day programs, and other support services to keep your parent home, you can compare those costs directly to full-time memory care. Sometimes the numbers look surprisingly similar, especially when you factor in your own lost income from reduced work hours or the toll on your health requiring your own medical care.
The decision to transition from respite to permanent placement rarely feels easy, even when it makes logical sense. Guilt runs deep for many adult children. You promised you'd never put Mom in a home. You feel like you're giving up or abandoning her. These emotions are normal, but they shouldn't override practical assessment of what your parent truly needs and what you can realistically provide.
Some families use a series of respite stays as a gradual transition. Your parent spends one week per month in memory care, then two weeks, then moves to permanent placement when everyone's adjusted. This approach can ease the emotional difficulty while giving your parent time to become familiar with the environment and staff.
Consider speaking with the memory care staff honestly about what you're observing. They can help you evaluate whether permanent placement makes sense based on your parent's needs, behaviors, and response to professional care. They've seen hundreds of families navigate this transition and can offer perspective without judgment.
Cost Comparison: Running the Numbers
Understanding the true cost difference between respite care and permanent memory care requires looking beyond monthly fees to examine what you're actually getting for your money and what hidden costs exist in each option.
Respite Care Costs (as of 2025)
In-home respite care averages $35 per hour nationally, though rates range from $15 to $40 depending on your location and the caregiver's experience level. If you need overnight coverage, expect to pay for 8 to 12 hours even if your parent sleeps through most of it. A weekend of respite (48 hours) could cost $1,400 to $1,900 for continuous care.
Adult day programs cost approximately $103 per day on average. Using this option three days per week runs about $1,200 per month. These programs typically operate during business hours only, so you'll need other coverage for evenings, nights, and weekends.
Facility-based respite care at memory care communities costs around $200 per night for specialized dementia care, or $1,400 per week. Some facilities charge $150 to $175 per day for respite in assisted living settings. These rates usually include meals, activities, and 24-hour supervision. Most communities require minimum stays of three to five days and may charge admission fees or assessment costs even for short-term stays.
Nursing home respite care runs higher, typically $200 to $300 per day depending on the level of medical care needed. This translates to $1,400 to $2,100 per week.
Memory Care Costs (as of 2025)
Permanent memory care costs vary significantly by location, but national averages provide useful benchmarks. The median monthly cost ranges from $6,450 to $7,785 depending on the source and region. This breaks down to approximately $215 to $260 per day.
These monthly fees typically include a comprehensive package: private or shared bedroom, all meals and snacks, 24-hour staffing and supervision, assistance with activities of daily living, medication management, laundry and housekeeping, secured environment to prevent wandering, specialized dementia activities and programming, emergency response systems, and basic health monitoring.
What memory care doesn't usually include: additional charges for higher levels of care (often $500 to $2,000 more per month as needs increase), medication costs and pharmacy fees, incontinence supplies, personal items and toiletries, beauty and barber services, transportation to medical appointments outside the facility, and specialized therapies like physical therapy or speech therapy.
The Real Comparison
Here's where the math gets interesting. If you're currently cobbling together home care to avoid placement, you might already be spending amounts comparable to memory care. Consider this scenario:
Adult day program three days per week: $1,200 Home health aide 20 hours per week for coverage gaps: $2,800 Overnight monitoring service two nights per week: $1,000 Your lost income from reduced work hours: $1,500 Monthly total: $6,500
That's approximately the same cost as memory care, except you're still providing the majority of care yourself, you're exhausted, and you're covering only partial supervision. There's no night coverage most nights, no backup when the home health aide calls in sick, and no specialized dementia training for most helpers.
Medicare provides extremely limited respite coverage. Original Medicare Part A covers respite care only for hospice patients, up to five consecutive days at a time in an approved inpatient facility. Medicare pays 95% of the cost, leaving you responsible for 5% coinsurance. This benefit helps families facing end-of-life care but doesn't apply to ongoing dementia care for someone not in hospice.
Medicaid coverage for respite care varies significantly by state. Many states offer some respite services through Home and Community-Based Services (HCBS) waiver programs, but availability, eligibility requirements, and covered services differ. Contact your state Medicaid office to learn what's available in your area.
Veterans may qualify for respite care through VA benefits. Eligible veterans can receive up to 30 days per year of respite care through VA programs. Services may be provided at home, in adult day health care centers, or in VA Community Living Centers. The Program of Comprehensive Assistance for Family Caregivers (PCAFC) offers up to 30 days of annual respite care along with caregiver stipends ranging from approximately $1,800 to $3,000 per month for qualified veterans with service-connected disabilities.
Long-term care insurance may cover both respite care and memory care, depending on your policy terms. Review your policy carefully to understand daily benefit amounts, elimination periods, and lifetime maximums.
Coverage and Payment Options
Most families pay for respite care and memory care privately, at least initially. Medicaid becomes an option for memory care once your parent's assets are spent down to qualification levels, typically around $2,000 in countable assets depending on your state. Many memory care communities accept Medicaid after a period of private pay, though availability of Medicaid beds may be limited.
Some memory care communities offer respite care rates that serve as a trial before permanent placement. If your parent transitions to full-time residency, some facilities credit part or all of the respite fees toward the first month's payment or the community fee.
Ask about all-inclusive pricing versus tiered care levels. Some communities charge one flat monthly rate regardless of care needs. Others use a base rate plus additional charges as your parent's needs increase. Understanding the pricing structure helps you budget accurately and avoid surprise costs.
Signs Permanent Placement Makes More Sense
Several indicators suggest your parent needs more than occasional respite care. Wandering behaviors that put safety at risk signal the need for secured memory care environments. If your parent has gotten lost in the neighborhood, tried to drive when no longer capable, or attempted to leave home at odd hours, professional supervision becomes necessary.
Aggressive behaviors during personal care, whether toward you or paid caregivers, often improve in professional memory care settings. Staff trained in dementia care use specific techniques to reduce resistance and maintain dignity. They don't have the emotional history that complicates family caregiving relationships.
Your own health deteriorating from caregiver stress indicates unsustainable circumstances. Depression, anxiety, physical illness, and relationship problems with other family members all suggest you need more than temporary respite. Permanent placement isn't giving up, it's recognizing limits and choosing the best care option available.
Advanced dementia stages require professional oversight. When your parent needs help with most or all activities of daily living, requires medication management beyond your training, or has medical needs you can't safely handle, memory care provides appropriate support levels.
Using Respite Care Strategically
Even if your parent doesn't need permanent memory care yet, strategic use of respite care protects your health and sustainability as a caregiver. Regular respite, even just a few hours weekly, prevents burnout better than waiting until you're in crisis.
Schedule respite care in advance rather than only for emergencies. Knowing you have reliable breaks coming helps you manage stress. Many adult day programs and home care agencies offer regular schedules, providing consistency for both you and your parent.
Use longer respite stays to evaluate whether your parent might benefit from memory care. A one-week stay gives you both a realistic preview. Your parent experiences the environment, activities, and care approach. You observe their response and gain perspective on your caregiving situation.
Consider respite care during high-stress periods. If you're recovering from surgery, dealing with work demands, or facing family crises, respite care prevents your parent's care from suffering while you handle other priorities.
Making the Decision
There's no perfect formula for deciding between continued respite care and permanent memory care placement. The decision depends on your parent's needs, your capacity as a caregiver, financial resources, and what will provide the best quality of life for everyone involved.
Start by honestly assessing the current situation. Document what's working and what's not. Track incidents that concern you regarding safety, behavior, or care needs. Note your own physical and mental health status. This information helps you evaluate options objectively.
Tour memory care communities even if you're not ready for placement. Seeing what professional memory care actually looks like, meeting staff, and understanding their care approaches provides valuable information for future decisions. Many families wish they'd toured earlier, before crisis forced rushed choices.
Talk with your parent's doctor about their current and anticipated needs. Physicians can provide perspective on disease progression and care requirements you might not fully recognize.
Connect with other family members who provide care or have input into decisions. Sharing the assessment process and decision-making reduces conflict and helps everyone understand the reasoning behind choices.
If guilt is your primary obstacle to considering memory care, remember this: choosing professional care when needed demonstrates love and wisdom, not abandonment. Your parent deserves safe, competent care from people trained to provide it. You deserve a life that includes rest, health, and relationships beyond caregiving.
Sometimes the best choice is the one you resist most. When respite stays consistently show your parent thriving in professional care, and you return home each time wondering how to keep going, those are meaningful signals worth acknowledging.
Moving Forward
Whether you choose continued respite care, transition to permanent memory care, or some combination of both, the goal remains the same: ensuring your parent receives appropriate care while preserving your own wellbeing.
Respite care serves an important role for families managing early to moderate dementia at home. It provides breaks that sustain home caregiving and prevents burnout that leads to hasty decisions. Use it strategically and regularly, not just in emergencies.
Memory care offers specialized support that most families can't replicate at home, regardless of dedication and love. When dementia progresses to the point where your parent needs professional oversight, making that transition reflects good judgment, not failure.
Many families find peace in knowing their parent is safe, cared for by trained professionals, and participating in activities appropriate for their cognitive level. The relief from constant worry often improves the quality of your visits, allowing you to be a loving daughter or son rather than an exhausted caregiver.
You'll make the right decision for your family's situation. Start by gathering accurate information about both respite care and memory care options, honestly assess your current circumstances, and don't let guilt override practical wisdom about what your parent truly needs.