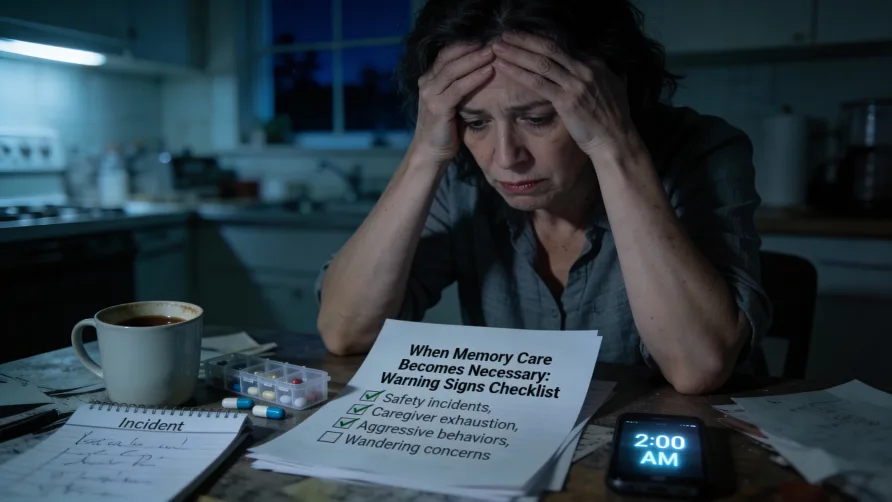
The police officer stood on Jennifer's porch at 2:30 a.m. holding her father's arm. Dad wore his pajamas and one slipper. He'd made it four blocks from the house before a neighbor spotted him trying to get into a car that wasn't his. "He kept saying he needed to get to work," the officer explained. "That he was late for his shift."
Dad hadn't worked for years. He retired 15 years ago. . But somewhere in his mind, confused by Alzheimer's, he was still a young man with responsibilities and a job to get to.
This wasn't the first incident. Jennifer had installed extra locks on the doors after Dad wandered into a neighbor's house at dinner time. She'd put bells on the bedroom door so she'd hear if he tried to leave at night. She barely slept anymore, listening for sounds of movement. Her husband had started sleeping in the guest room because her nighttime vigilance kept him awake too.
As the officer left, Jennifer stood in her kitchen crying. She'd promised her mother before she died that she'd never put Dad in a home. She loved him. She wanted to care for him. But how could she keep doing this? What if the next wandering incident ended differently? What if no one found him?
This moment, when safety overrides everything else, happens in thousands of families every year. You reach a point where love and determination aren't enough to keep your parent safe at home.
Family Decision Note
Deciding when to move a loved one to memory care involves medical, legal, and emotional considerations unique to your family. While we share what typically happens and what to consider, always involve your parent's healthcare team in these decisions. We're here to inform, not to replace professional medical guidance.
Recognizing When Home Care Isn't Enough
Memory care provides specialized residential support for people with Alzheimer's disease and other forms of dementia. These communities offer 24-hour supervision, secured environments to prevent wandering, staff trained in dementia care techniques, and structured activities designed for cognitive impairment.
The decision to transition from home care to memory care ranks among the most difficult choices adult children face. You want to honor your parent. You feel guilty considering placement. You worry about how they'll react.
But certain signs indicate your parent needs more support than you can safely provide at home, regardless of how much you love them or how hard you try. These warning signs reflect the progressive nature of dementia and the point where professional oversight becomes necessary.
Sign 1: Wandering That Puts Safety at Risk
Wandering represents one of the most urgent reasons families move parents to memory care. According to the Alzheimer's Association, 60% of people with dementia will wander at least once, and many do so repeatedly.
Your parent gets up at 3 a.m. dressed in winter clothes because they think they need to pick up the kids from school. The kids are adults now with their own children, but that reality doesn't register anymore. They head for the door while you're sleeping. By the time you discover they're gone, they could be blocks away, confused and vulnerable.
Or perhaps your parent has started "going home" even when they're already in their own house. They don't recognize the place they've lived for 30 years. The environment feels foreign and frightening. They try to leave, looking for the home they remember from decades earlier.
Wandering isn't just about getting lost outside. Your parent might wander within the house at night, becoming disoriented about which room is the bathroom. They might try to cook at odd hours, turn on the stove and forget about it, or attempt to drive when they haven't been capable in years.
What families often underestimate is how quickly safety becomes an issue once wandering starts. You can install locks and alarms. You can create elaborate security systems. You can sleep with one ear always listening. But eventually, exhaustion catches up with you. You fall asleep deeply just once, and that's when your parent walks out the door into freezing weather or busy traffic.
Memory care communities have secured environments specifically designed for people with dementia who wander. Doors have delayed-exit alarms. Outdoor areas are enclosed and safe. Staff members monitor residents around the clock. Your parent can move freely within safe boundaries rather than being constantly restrained or locked in a bedroom at home.
The guilt feels crushing when you acknowledge you can't prevent wandering safely at home anymore. But memory care doesn't mean giving up. It means providing the level of safety your parent's condition now requires.
Sign 2: Aggressive or Combative Behavior During Personal Care
Your mother has always been gentle and kind. But when you try to help her shower, she hits you. When you attempt to change her clothes, she screams that you're attacking her. When you give her medications, she spits them out and accuses you of poisoning her.
This behavior, called care resistance, devastates families emotionally. The parent you've known your whole life suddenly treats you like a threat. You're trying to help them stay clean, comfortable, and healthy, but they perceive your assistance as assault.
Care resistance happens because dementia damages your parent's ability to understand what's happening. They don't recognize you anymore. They don't understand why a stranger is touching them, removing their clothing, or trying to make them do things. From their confused perspective, they're defending themselves against danger.
The situation becomes physically unsafe when your parent's resistance turns aggressive. They might push, hit, bite, or scratch. Even if they're small and elderly, their fear-driven strength can cause injury. You start avoiding necessary care tasks because they're too difficult and upsetting for everyone involved. Your parent's hygiene deteriorates. Medication schedules slip. Their health declines because you can't provide the care they need.
Memory care staff members are trained in dementia-specific care techniques that reduce resistance. They approach personal care differently than family members do. They use specific communication methods, environmental cues, and caregiving sequences that minimize anxiety and confusion. Separating the caregiver role from the family relationship often reduces aggressive behaviors significantly.
The professional staff also work in teams. If one person struggles to assist your parent with showering, another team member can step in with a different approach. They have the training, experience, and emotional distance to handle care resistance without taking it personally or becoming burned out.
When aggressive behavior makes personal care impossible at home, memory care provides the structure and expertise needed to maintain your parent's dignity and health.
Sign 3: You've Become Isolated, Exhausted, and Your Health Is Failing
You haven't seen your friends in months. You've used up all your vacation days and sick leave for caregiving. Your spouse feels like a roommate because you're too exhausted for conversation. Your kids complain they never see you anymore, even though you live in the same house. You've gained weight, developed high blood pressure, and your doctor keeps telling you that you need to reduce stress.
Caregiver burnout doesn't happen suddenly. It creeps up gradually as caregiving demands increase and your own needs get pushed aside. You skip doctor appointments because you can't leave your parent alone. You stop exercising because you don't have energy. You live on fast food because cooking feels impossible. You cry over small things because your stress tolerance is completely depleted.
Maybe you've developed depression or anxiety. You wake up dreading the day ahead. You fantasize about getting in your car and driving away. Then you feel horrible guilt for having those thoughts because you love your parent and want to care for them.
The problem is that your parent's needs are now 24/7. Dementia doesn't take breaks. Your parent needs supervision every hour of every day. Even when you hire help, you're still managing schedules, solving problems, handling emergencies, and carrying the mental load of being responsible for another adult's complete wellbeing.
Your health matters. If you get sick, injured, or have a breakdown, who will care for your parent then? The emergency placement that happens when a caregiver collapses is far worse than a planned, thoughtful transition to memory care.
Memory care allows you to return to being a son or daughter rather than an exhausted, burned-out caregiver. You can visit, spend quality time, participate in activities together, and actually enjoy your parent's company again instead of feeling constantly overwhelmed by their care needs.
This isn't giving up. It's recognizing that you're human with real limits, and that professional care provides support you cannot replicate alone at home.
Sign 4: Medication Management Has Become Dangerous
Your parent takes eight different medications with complex schedules. Some are twice daily, others three times daily, one is every other day. Your parent forgets whether they've taken their pills. They take double doses, skip doses entirely, or mix up medications. You've found pills hidden in drawers, stuffed in couch cushions, or dissolved in the bathroom sink.
When you try to manage medications yourself, your parent resists. They insist they don't need the pills, that you're trying to drug them, or that the medications are making them sick. They refuse to swallow pills you've watched them take happily for years.
The consequences of medication errors with dementia patients can be serious. Blood pressure medications skipped or doubled cause dangerous fluctuations. Diabetes medications missed or duplicated lead to emergency situations. Blood thinners mismanaged create stroke or bleeding risks.
Memory care communities provide professional medication management. Staff members administer medications on schedule, document what's given, and monitor for side effects. Your parent receives the right medications at the right times without confusion, resistance, or dangerous errors.
Sign 5: They Can No Longer Be Left Alone Safely
You used to run quick errands while your parent watched television. Now you can't leave them alone for five minutes. They might turn on the stove and forget about it. They might try to leave the house. They might fall and not be able to get up.
You've tried hiring home health aides, but your parent refuses to let them in, becomes agitated with strangers in the house, or waits until the aide is in the bathroom to do something dangerous. The supervision needs are constant and unrelenting.
This sign usually appears gradually. First, you can't leave your parent alone for several hours. Then you can't leave them alone for an hour. Eventually, you realize they need someone physically present every moment, including overnight. That level of supervision is nearly impossible to provide at home without destroying your own health and life.
Memory care provides continuous oversight. Staff members are always present. Your parent is never alone, never in danger from their own confusion or impaired judgment.
Sign 6: Basic Self-Care Has Broken Down Completely
Your parent refuses to bathe, change clothes, or use the toilet properly. They wear the same outfit for days despite your attempts to change them. They've developed urinary tract infections from poor hygiene. Their teeth are decaying because they won't brush them or let you help.
The environment suffers too. Your parent hoards food in their bedroom until it rots. They become incontinent but hide soiled clothing. They no longer maintain any basic cleanliness standards.
This deterioration affects their health, dignity, and your ability to keep the home environment safe and sanitary. Memory care staff handle personal hygiene as a routine part of daily care, using trained techniques to gain cooperation and maintain dignity even when the person with dementia resists.
Sign 7: You're Calling 911 Frequently
Emergency room visits have become regular occurrences. Your parent falls and you can't get them up safely. They have behavioral outbursts you can't calm. They refuse to eat for days and you panic. The paramedics know your address by heart. These frequent crises indicate care needs beyond home management. Memory care facilities have staff trained to handle medical emergencies and behavioral issues without requiring 911 calls for situations they can manage professionally.
Sign 8: Sundowning Makes Evenings and Nights Unmanageable
Your parent becomes increasingly confused, agitated, or aggressive as evening approaches. They pace, yell, try to leave, or become paranoid and frightened. This sundowning behavior makes nights impossible. You can't sleep because your parent is awake and agitated for hours. Memory care environments use specialized lighting, structured routines, and trained staff to minimize sundowning effects and keep residents safe during vulnerable evening hours.
Sign 9: They No Longer Recognize Family Members
Your parent looks at you blankly. They don't know who you are. They call you by their sibling's name or think you're a stranger who broke into their house. This lack of recognition is emotionally devastating, but it also creates safety issues because your parent doesn't trust you or accept care from you. Professional caregivers in memory care become familiar, trusted figures even when family members are no longer recognized.
Sign 10: Their Doctor Recommends Higher-Level Care
Your parent's physician has directly stated they need memory care. The doctor has explained that your parent's condition requires professional oversight you can't provide at home. Medical professionals see the clinical progression and safety risks objectively. When a doctor recommends memory care, they're telling you that home care has become inadequate for your parent's needs. This professional assessment should carry significant weight in your decision-making.
What Families Often Underestimate
Safety deteriorates faster than most families expect. The wandering incident that happens once becomes three times a week. The medication error that seemed minor leads to a hospitalization. The fall that didn't cause injury the first time breaks a hip the second time.
Families often wait too long, managing increasingly dangerous situations at home until a crisis forces emergency placement. This rushed decision-making under stress leads to poor outcomes. You choose whichever facility has an opening right now rather than thoughtfully selecting the best community for your parent's needs.
Starting the conversation about memory care before crisis hits gives you time to research options, tour communities, understand costs, and involve your parent in the decision-making process to whatever degree their cognitive function allows. You make better choices when you're not operating in emergency mode.
The progression of dementia doesn't reverse. These signs indicate your parent has reached a stage where professional care provides safety and quality of life that home care cannot match. Recognizing these signs early allows for better planning and smoother transitions.
Taking the Next Step
If you recognize multiple signs on this list, it's time to have serious conversations with your parent's doctor, other family members involved in care decisions, and memory care communities in your area.
Schedule tours at memory care facilities. See what these environments actually look like. Talk with staff members about their training and approaches. Ask about admission criteria, costs, and services provided. Watch how staff interact with residents. Notice whether residents seem content, engaged, and safe.
Involve your parent's physician in the discussion. Ask for their clinical assessment of whether memory care is now appropriate. Request specific input on your parent's safety risks and care needs.
Talk with family members about the decision. Share the responsibility and reasoning. Address concerns and objections openly. Make sure everyone understands the factors driving this difficult choice.
If financial concerns are holding you back, explore payment options. Many families don't realize that long-term care insurance, veterans benefits, or eventual Medicaid coverage might help with memory care costs.
Remember that this decision reflects love, not abandonment. You're choosing the environment where your parent can be safest, receive appropriate care, and maintain the best possible quality of life given their condition. That's what good caregiving looks like when dementia progresses beyond what any family can manage alone at home.