Vascular dementia accounts for 15 to 20% of all dementia cases in North America and Europe, making it the second most common form of dementia after Alzheimer's disease. Yet diagnostic confusion remains surprisingly common. Studies show that up to 60% of people with dementia have evidence of vascular brain disease, but many never receive an accurate vascular dementia diagnosis. This matters because the care approach should be different.
If your parent was diagnosed with vascular dementia, you're probably discovering that not all memory care facilities understand what makes this condition unique. Some treat it exactly like Alzheimer's disease. Others recognize the differences in theory but don't actually adapt their care protocols. Finding memory care that addresses vascular dementia's specific patterns and needs requires knowing what questions to ask and what specialized support should look like.
What Vascular Dementia Actually Is
Vascular dementia develops when brain cells don't receive enough oxygen and nutrients due to damaged blood vessels. This happens most commonly after strokes, either major strokes that produce obvious symptoms or series of small strokes that may go unnoticed. It can also result from conditions that damage small blood vessels throughout the brain, reducing blood flow gradually over time.
The key difference from Alzheimer's disease is that vascular dementia stems from cardiovascular problems rather than protein buildups in the brain. This means your parent's brain health is directly connected to their heart and vascular health. Managing blood pressure, cholesterol, diabetes, and other cardiovascular risk factors isn't just general health maintenance. It's dementia treatment.
Vascular Dementia vs. Alzheimer's Care Differences
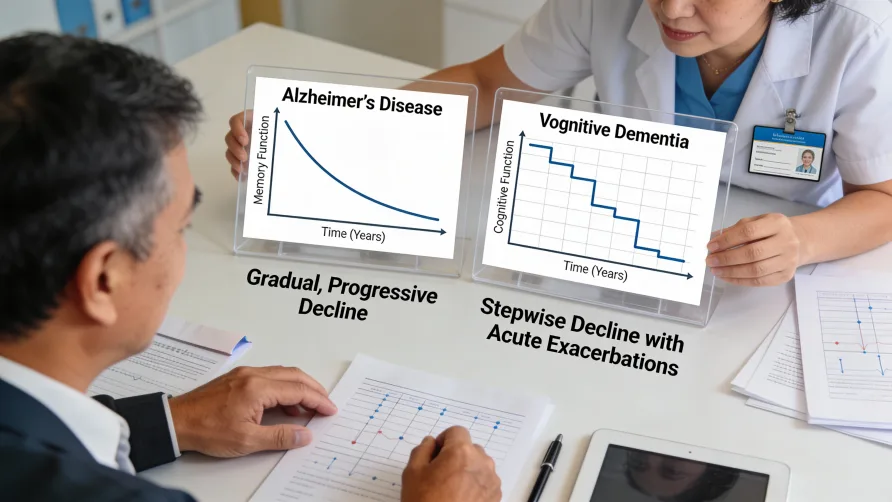
Where this gets confusing is that vascular dementia and Alzheimer's disease can look similar on the surface. Both cause memory problems, both progressively worsen, and both eventually require full-time care. But the patterns differ in ways that should change how care is delivered.
The progression patterns are fundamentally different. Alzheimer's disease typically follows a gradual, steady decline. Your parent gets a little worse each month, but the changes are often subtle day to day. Vascular dementia progresses through steps. Your parent might function at a fairly stable level for weeks or months, then experience a sudden drop in abilities following a stroke or vascular event. After that drop, they may plateau again at this new, lower level of function. This stepwise pattern is so characteristic that doctors call it the hallmark of vascular dementia.
This difference in progression means care planning has to work differently. With Alzheimer's, you can usually see changes coming gradually and adjust care incrementally. With vascular dementia, you might think your parent is doing relatively well, then face a medical crisis that suddenly changes everything. Memory care facilities experienced with vascular dementia build in flexibility for these sudden shifts and maintain close coordination with medical providers to respond quickly when vascular events occur.
The symptoms appear in a different order. Alzheimer's disease typically begins with memory problems. Your parent forgets recent conversations, misplaces items, and has trouble remembering appointments. Executive function problems like difficulty with planning and decision-making come later. Vascular dementia often works in reverse. The first noticeable symptoms might be slower thinking, trouble following conversations, difficulty making decisions, and problems with planning or organizing tasks. Memory can remain relatively preserved in early stages.
This matters for daily care. Someone with vascular dementia might remember conversations from yesterday but struggle to figure out how to get dressed or what steps are needed to make coffee. They need different types of support than someone whose primary challenge is memory loss. Activities and therapy approaches should target executive function, attention, and processing speed rather than focusing heavily on memory aids.
Physical symptoms appear earlier and more prominently. People with Alzheimer's typically maintain physical abilities through middle stages of the disease. Walking, coordination, and motor skills stay relatively intact even as memory and thinking decline. Vascular dementia often causes physical changes early. Your parent might develop a shuffling gait, have trouble with coordination, experience weakness on one side of their body, or show other neurological symptoms depending on where stroke damage occurred in the brain.
Memory care staff working with vascular dementia patients need training in recognizing and responding to physical changes that signal new vascular events. Sudden changes in walking ability, increased falls, new weakness, or speech difficulties aren't just normal progression. They're medical emergencies requiring immediate evaluation.
Mixed dementia is extremely common. Here's what complicates everything: pure vascular dementia is actually rare. Autopsy studies show that only about 10 to 15% of people diagnosed with vascular dementia have damage from strokes alone. The majority have both vascular damage and Alzheimer's disease pathology. Some estimates suggest mixed dementia may be the most common form of dementia in older adults.
This means your parent's care needs to address both conditions. They might need memory support strategies typical of Alzheimer's care alongside the cardiovascular risk management and stepwise progression monitoring typical of vascular dementia care. Facilities that truly understand vascular dementia recognize this overlap and don't treat it as purely one condition or the other.
Cardiovascular management is part of dementia treatment. This is perhaps the biggest difference. With Alzheimer's disease, managing blood pressure and cholesterol is general health maintenance. With vascular dementia, controlling cardiovascular risk factors is dementia treatment aimed at preventing further brain damage.
Memory care facilities specializing in vascular dementia maintain close relationships with cardiology and primary care providers. They monitor blood pressure regularly, ensure medications for hypertension, diabetes, and high cholesterol are taken correctly, and watch for signs of new cardiovascular events. When your parent's blood pressure isn't controlled or their diabetes management slips, that's not just a medical problem. It's an immediate threat to their cognitive function.
What Specialized Vascular Dementia Care Looks Like
Memory care that genuinely addresses vascular dementia builds several specialized elements into their approach.
Medical oversight focuses on stroke prevention. Staff should monitor vital signs more frequently than standard memory care requires. Blood pressure checks happen regularly, not just during routine medical appointments. The facility maintains protocols for recognizing stroke symptoms quickly, even subtle changes that might indicate small vessel disease. They know the signs: sudden confusion, new trouble speaking, facial drooping, arm weakness, difficulty walking, severe headache, or sudden vision changes.
Medication management receives extra attention. Medications that control blood pressure, prevent blood clots, manage diabetes, and reduce cholesterol are considered critical, not optional. Staff understand that missed doses directly increase stroke risk and cognitive decline risk.
Care plans adapt to stepwise changes. Rather than assuming steady, predictable decline, care planning accounts for the possibility of sudden function loss. The facility has protocols for rapid assessment and care plan adjustment when residents experience vascular events. They work closely with families to ensure medical decision-making happens quickly when your parent's condition changes suddenly.
Activity programs recognize that executive function problems might be your parent's primary challenge. They structure activities with clear, simple steps and provide the organizational support vascular dementia patients need. Staff understand that someone who can't plan a task sequence might still engage fully if someone else provides the structure.
Physical therapy and mobility support start early. Because physical symptoms often appear sooner in vascular dementia, facilities may incorporate more physical and occupational therapy services. Staff receive training in safe transfers and movement support for residents who have had strokes. The physical environment accommodates mobility aids and accounts for balance problems or one-sided weakness.
General Memory Care Fundamentals
Like all memory care, facilities serving vascular dementia patients provide secure environments, assistance with daily activities including bathing, dressing, and medication management, and programs designed to maintain remaining abilities. Staff-to-resident ratios allow for individualized attention. The environment is designed to support independence while ensuring safety. Social engagement and meaningful activities remain central to maintaining quality of life, even as abilities decline.
However, these baseline memory care services aren't enough for vascular dementia. The condition requires the additional layers of cardiovascular monitoring, stroke recognition, and adaptation to stepwise progression that many standard memory care programs don't provide.
Questions That Reveal Vascular Dementia Expertise
When evaluating memory care facilities, ask questions that expose whether they understand vascular dementia's unique patterns.
How do you handle cardiovascular risk factor management? Listen for specifics about blood pressure monitoring frequency, coordination with cardiologists or primary care doctors, and protocols for ensuring cardiovascular medications are taken correctly. If they talk about this as just following doctor's orders rather than recognizing it as dementia treatment, they may not fully understand vascular dementia.
What happens when a resident experiences a stroke or vascular event? You want to hear about rapid assessment protocols, immediate medical coordination, and systems for quickly adjusting care plans. Facilities experienced with vascular dementia have these procedures in place because they understand stepwise decline is the norm, not an unexpected crisis.
How is vascular dementia care different from Alzheimer's care in your facility? This question reveals whether they actually differentiate between the conditions or treat all dementia as essentially the same. Look for answers that mention cardiovascular management, stroke monitoring, executive function support, and flexibility for sudden changes.
What training do staff receive specific to vascular dementia? General dementia training isn't enough. Staff should receive education about recognizing stroke symptoms, understanding stepwise progression, supporting executive function difficulties, and coordinating medical care focused on preventing further vascular damage.
How do you work with residents who have mixed dementia? Most people with vascular dementia actually have mixed pathology. Facilities should acknowledge this and explain how they address both vascular and Alzheimer's components rather than treating the diagnosis as either/or.
Signs a Facility Doesn't Understand Vascular Dementia
Red flags suggest a facility treats vascular dementia as just another form of memory loss without addressing its specific needs.
They talk about dementia as if all types are the same and don't differentiate their care approaches. They can't articulate what makes vascular dementia care different from Alzheimer's care beyond saying they "follow the doctor's treatment plan."
Blood pressure monitoring happens only during scheduled medical appointments rather than regularly throughout the week. Staff can't explain their stroke recognition protocols or what happens when they notice sudden changes in a resident's function or behavior.
Care plans look identical regardless of dementia type. Activities focus almost exclusively on memory support without addressing executive function, attention, or processing speed challenges that are often primary in vascular dementia.
They don't mention coordination with cardiology or emphasis on cardiovascular medication compliance. Medical oversight appears minimal beyond basic medication administration.
What About Mixed Dementia?
If doctors have told you your parent has mixed dementia (both vascular dementia and Alzheimer's disease), the facility needs to address both conditions. This means combining the memory support, cognitive stimulation, and structured routine beneficial for Alzheimer's with the cardiovascular management, stroke prevention, and stepwise progression monitoring needed for vascular dementia.
Mixed dementia often results in faster overall decline than either condition alone. Research suggests that vascular damage and Alzheimer's pathology interact, with each making the other worse. Care should be more intensive than what either condition would require separately.
Cost Considerations
Memory care for vascular dementia typically costs the same as standard memory care, generally ranging from $4,000 to $8,000+ per month depending on location and level of care needed. The specialized services (increased medical monitoring, coordination with cardiovascular specialists, stroke protocols) should be included in base pricing rather than charged as add-ons.
However, be prepared for medical costs beyond the facility's monthly fee. Your parent may need frequent cardiology appointments, additional medications, and medical interventions to manage cardiovascular risk factors. These medical services typically aren't covered by memory care fees.
When Specialized Vascular Dementia Care Becomes Necessary
Consider specialized memory care when your parent's cardiovascular health and cognitive function are clearly connected, when strokes or vascular events have caused stepwise declines in abilities, when managing multiple cardiovascular medications has become complex, or when they need regular medical monitoring you can't provide at home.
The decision often crystallizes after a stroke or vascular event reveals that previous care arrangements can't accommodate sudden function changes. Other families recognize the need when cardiovascular risk factors aren't being adequately controlled at home, putting their parent at risk for additional brain damage.
The Reality of Vascular Dementia Prognosis
Vascular dementia typically has a shorter life expectancy than Alzheimer's disease. Published research notes a range of three to five years from diagnosis, though this varies considerably based on overall cardiovascular health and whether additional strokes occur. The condition is ultimately terminal, with most people dying from cardiovascular events like heart attacks or strokes rather than from dementia complications directly.
This difficult reality means care should focus on quality of life, cardiovascular health to prevent additional strokes, and ensuring your parent receives appropriate medical intervention when vascular events occur. End-of-life planning becomes important earlier in the disease course because sudden changes can happen without warning.
Making the Choice
Vascular dementia requires memory care that understands cardiovascular disease is driving the cognitive decline. Your parent needs more than supervision and dementia-appropriate activities. They need medical oversight focused on preventing additional strokes, care plans built to adapt quickly when function changes suddenly, and staff who recognize that controlling blood pressure and managing diabetes is protecting brain function.
Not every memory care facility delivers this level of specialized support. The label "memory care" doesn't guarantee vascular dementia expertise any more than it guarantees specific Alzheimer's training. You have to ask detailed questions, observe how facilities actually operate, and verify that their care approach matches what vascular dementia requires.
When you find memory care that truly understands vascular dementia, you see the difference in how they monitor your parent's cardiovascular health, how quickly they respond to changes, and how they balance supporting current function with preparing for stepwise declines. That specialized understanding matters enormously for both immediate quality of care and long-term outcomes.